Global Antimicrobial Resistance Deaths Projected to Rise by 70% by 2050, New Study Warns
In a recent study published in the journal The Lancet, researchers project that worldwide deaths caused by infections resistant to treatment could surge nearly 70% by 2050. The study highlights the escalating challenge posed by antimicrobial resistance (AMR).
The analysis indicates that between 2025 and 2050, more than 39 million deaths could be attributed to antimicrobial resistance, reflecting the significant global health crisis it represents.
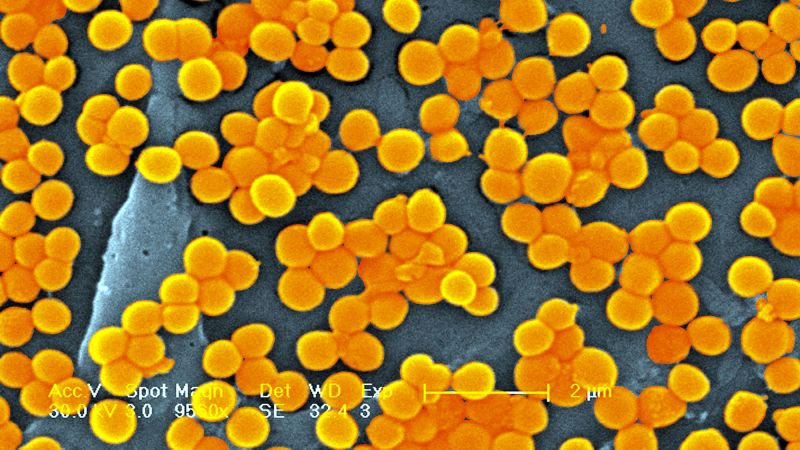
Antimicrobial resistance arises when microbes, including bacteria and fungi, evolve to evade the medications designed to eradicate them. The World Health Organization (WHO) has identified AMR as “one of the top global public health and development threats,” emphasizing concerns over the misuse and overuse of antimicrobial drugs in humans as well as in animal and agricultural practices.
Dr. Chris Murray, director of the Institute for Health Metrics and Evaluation at the University of Washington and the study’s lead author, expressed concern about the worsening trend, stating, “We expect it to get worse.” He urged for increased focus on developing new antibiotics and implementing antibiotic stewardship to combat this significant issue.
The research team, which included experts from the Global Research on Antimicrobial Resistance Project and various institutions, analyzed illness and mortality data linked to antimicrobial resistance across 22 pathogens and 84 pathogen-drug combinations in 204 countries and territories from 1990 to 2021. They distinguished between deaths directly caused by AMR and those that were exacerbated by it, relying on approximately 520 million individual health records for their estimates.
The findings reveal a decrease in AMR-related deaths among children under five, which fell by more than 50% from 1990 to 2021, while deaths among adults aged 70 and older increased by over 80%, a trend expected to persist. "We had these two opposite trends going on: a decline in AMR deaths under age 15, mostly due to vaccination, water and sanitation programs," Murray noted.
Additionally, the researchers highlighted methicillin-resistant Staphylococcus aureus (MRSA) as the pathogen-drug combination with the largest increase in mortality burden, observing that attributable deaths nearly doubled from 57,200 in 1990 to 130,000 in 2021.
Using statistical modeling, the researchers forecasted possible scenarios for 2050: without significant intervention, deaths from AMR could reach 1.9 million, with an additional 8.2 million deaths associated with AMR. Regions most affected would include South Asia, Latin America and the Caribbean, and sub-Saharan Africa, where access to quality healthcare remains limited.
Murray emphasized, “There are still, unfortunately, a lot of places in low-resource settings where people who need antibiotics are just not getting them.” He pointed out that basic medical supplies, such as oxygen, are frequently unavailable in these areas, complicating care for seriously ill patients.
Despite the harrowing forecasts, the study also highlights that improved healthcare access and the development of new antibiotics could have a significant impact. In an ideal scenario of enhanced healthcare, the researchers estimate that up to 92 million deaths could be averted between 2025 and 2050, while new antibiotic classes could prevent approximately 11 million deaths.
Samuel Kariuki of the Kenya Medical Research Institute described the study as providing a "comprehensive assessment" of the AMR crisis. However, he cautioned that the models do not take into account the possible emergence of new superbugs.
Dr. Steffanie Strathdee, an expert in global health sciences at the University of California San Diego, underscores the importance of the research, citing her personal experience with antimicrobial resistance when her husband nearly died from an infection resistant to conventional antibiotics.
Reflecting on her family’s ordeal, Strathdee noted, “I’m somebody who’s lived with antimicrobial resistance affecting my family for the last eight years.” Following extensive treatment, her husband recovered, which she attributes to advancements like phage therapy, an alternative that targets resistant bacteria.
The study calls for urgent investment and action to mitigate the growing threat of antimicrobial resistance globally, advocating for enhanced access to antibiotics, vaccines, clean water, and better healthcare conditions. “There is possible hope on the horizon,” Strathdee concluded, highlighting that scaling up effective interventions could lead to significant reductions in mortality in the future.